Last year saw the launch of The Departure Lounge, the Academy’s most ambitious public engagement project ever. Our aim was to initiate a public conversation on the topic of death and dying and to feed what we heard into the Academy’s policy work. We did that by opening an innovative installation in a shop in Lewisham. Read more about how we developed the project here, but here’s 5 things we learnt from starting conversations about the end of life.
1. Lots of people want to talk about death and dying, but they might not take the first opportunity you offer them
Participants in our poll were informed that the questions were on death and then given the opportunity to opt out of answering them. This meant that one in three participants chose not to answer the questions, before even knowing what they were.
However when we explored this further in the shop we discovered that when people started from an uncomfortable place and said they didn’t want to talk about death, they often came back and then wanted to talk about it.
We were regularly faced with people who said ‘Nah I don’t want to talk about that’, but then as they were walking away they’d turn back and say, ‘but I will just say…’ and then spend a good half hour or more talking with the team.
2. People don’t know much about dying
Even though people think about it a lot of the time they don’t really know what happens. Six in ten people who answered our poll felt they knew little or nothing about the final hours of life. The poll also revealed that those who know at least a little about what happens at the end of life are roughly as likely to get their information about what happens from TV documentaries (20%) as they are from medical professionals (22%). Interestingly, information from films, dramas and soaps (16%) also falls in the top 5 sources of information.
The most common sources of information comes from conversations with family and friends (42%) and of course personal experience of being with someone in the final hours/minutes of their life (33%)
New poll shows how little we know about dying
3. People are more comfortable talking about some stages of death then others
When talking about the ‘end of life’ people tended to focus on three different stages, and there was a hierarchy of comfort in talking about them. None are necessarily easy, but there are places or stages where people are more likely to go.
We found the easiest part for people to talk about was the bit that comes after death. Talking about funeral planning, getting things in order, doing active things to minimise the burden on those left behind and supporting them to cope with their grief and loss.
People often spoke proudly about having thought about these things, especially if they had made specific plans.
People were OK, but less comfortable talking about the decline into death, however long that might have been, but they could still talk about and think though things like getting a terminal diagnosis, how it might change the way they live their life and considering where their end of life care might be provided while still able to live life fairly normally. But from here people tended to jump straight back to the post death phase where they were more comfortable.
When talking about the end of life, people rarely spoke about the final days, hours or minutes. They struggled to talk about what their hopes or fears would be for themselves or a relative. People didn’t know what might happen physically as the body shuts down or how they might be cared for, which made it difficult for them to think about the role of medicine during that time.
4. People don’t really know about palliative care
Not many people had heard of palliative care and those who had were unsure how it is organised, where it might be delivered and what the benefits might be. There are lots of misconceptions and a worry that engaging with palliative care meant giving up, fast tracking to the end or signing up for a lesser quality of care. Even though people didn’t call it palliative care, they talked a lot about wanting what it delivers - joined up care around the emotional and practical aspects of dying.
| See our resource: End of life care: your guide to who, what and where |
And lastly, one of the biggest things we heard time and time again …
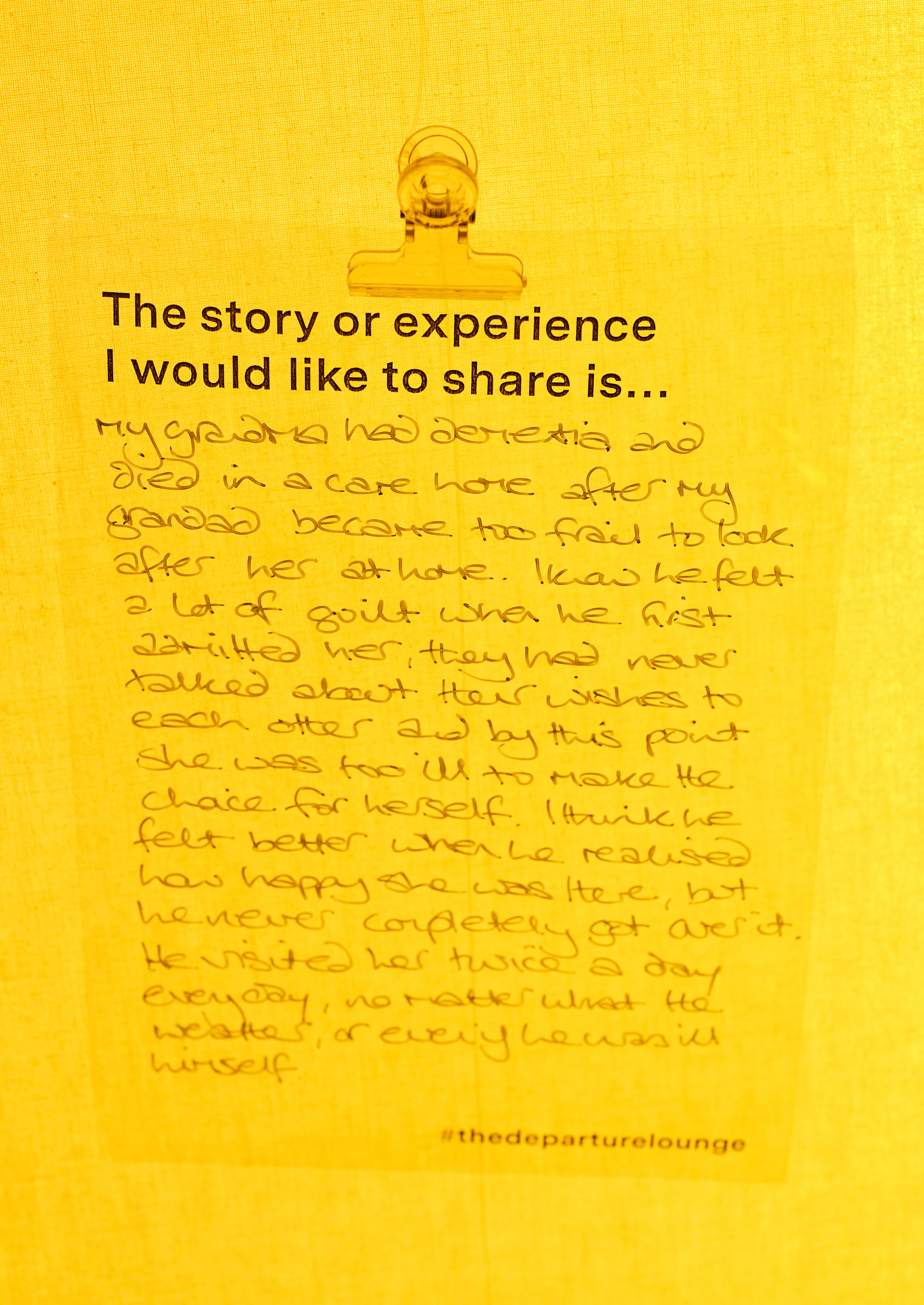
5. What matters most when you are living will matter most when you are dying.
The need to explore what matters to you and not what’s the matter with you was a really common theme when people talked about the end of life.
A good death for people was one that allowed them to be surrounded by the people they loved, doing the things they loved most for as long as possible (and preferably right up to their last breath!).
Very often this was about being able to have a glass of their favourite drink! But the underlying message of this was that their care needs to let that happen, even if it requires bending the rules just a little bit.
| Read our resource: 'Making decisions about your journey: helping you with end of life medical conversations' |
You can read more on what we learnt about death and dying from the Departure Lounge in the Ipsos Mori report ‘The Departure Lounge, Public attitudes to death and dying’, as well as anindependent evaluation for the project 'The Departure Lounge - Evaluation report'.
You can follow the discussion at #thedeparturelounge or visit us at www.departure-lounge.org
Funding for the project was received from Wellcome Trust and the Health Foundation and we are very grateful to them for their support.